Article
02 September 2024
Coarctation of the aorta is a frequently diagnosed congenital heart defect and
often requires surgical repair in early infancy. Infants born with this
condition remain at risk for post-operative morbidity and reintervention within
the first year of life. A single-center, retrospective chart review was
performed. The protocol was approved by the Institutional Review Board
(IRB-21-156, 14 August 2021). A 10-year review from January 2010 to
December 2020 identified all children diagnosed with coarctation of the aorta
or arch hypoplasia; without any associated major congenital cardiac pathology
(i.e., simple coarctation). Reintervention-free-survival at one year for all
infants who underwent surgical repair was assessed. Patient characteristics for
those who did and did not experience significant adverse event (SAE) in the
postoperative period were obtained and compared. A total of 105
patients diagnosed with isolated coarctation of the aorta or arch hypoplasia
and who underwent surgical repair were identified. Of these, 11 patients (10%)
experienced a SAE (i.e., vocal cord palsy, diaphragm palsy, chylothorax,
stroke/neurological complication, need for reintubation or tracheostomy,
necrotizing enterocolitis, major bleeding or thrombotic vascular complication,
or reintervention) in the post-operative period. Patients who experienced a SAE
were more likely to have a prenatal diagnosis of coarctation of the aorta (p =
0.03), a known genetic anomaly (p = 0.0001), or had undergone a median sternotomy
approach/complex arch repair (i.e., requiring
patching of the aorta) (p = 0.0001). Genetic anomaly (mainly Turner
syndrome) was the only independent predictor of SAE in multivariate analysis (OR
= 6.7) Follow up data at one year
was available for 79 patients, with only 6 patients requiring reintervention
before 1 year of age. Overall,
infants who undergo surgical repair of simple coarctation of aorta have an
excellent chance of reintervention-free-survival at one year post intervention.
Those with a known genetic anomaly or requiring median sternotomy approach appear
to have a higher risk for a SAE in the postoperative period.utf-8
ChristinaL.Benjamin
RooseveltBryant III
DeeptiP.Bhat
Research Highlight
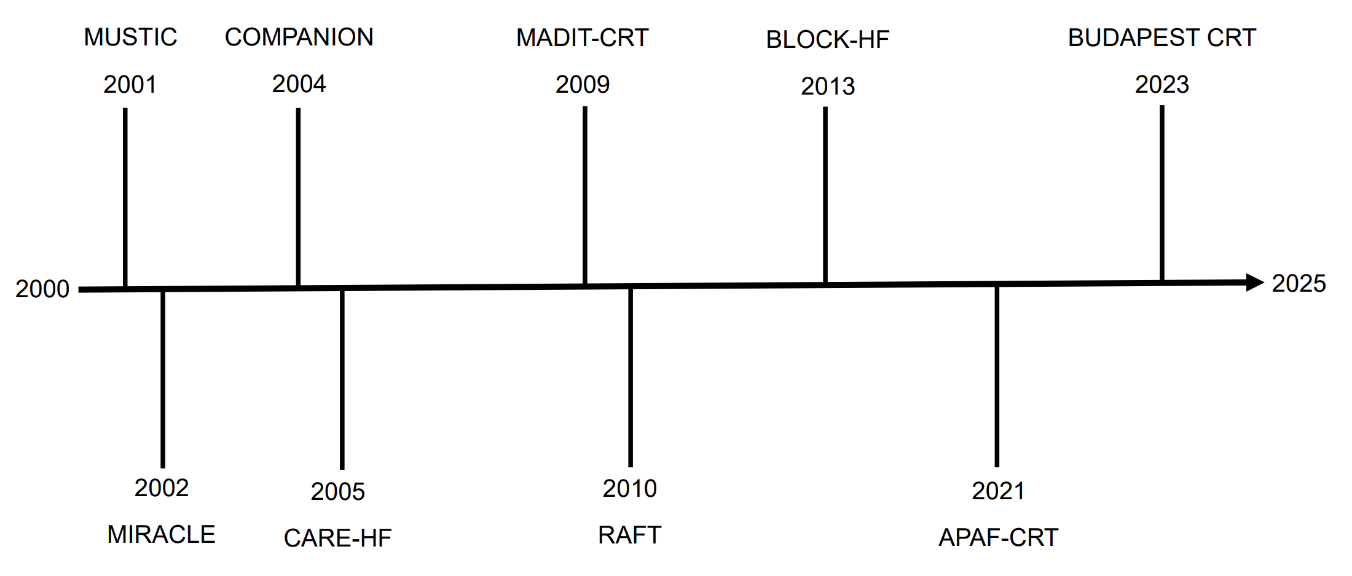
27 September 2024
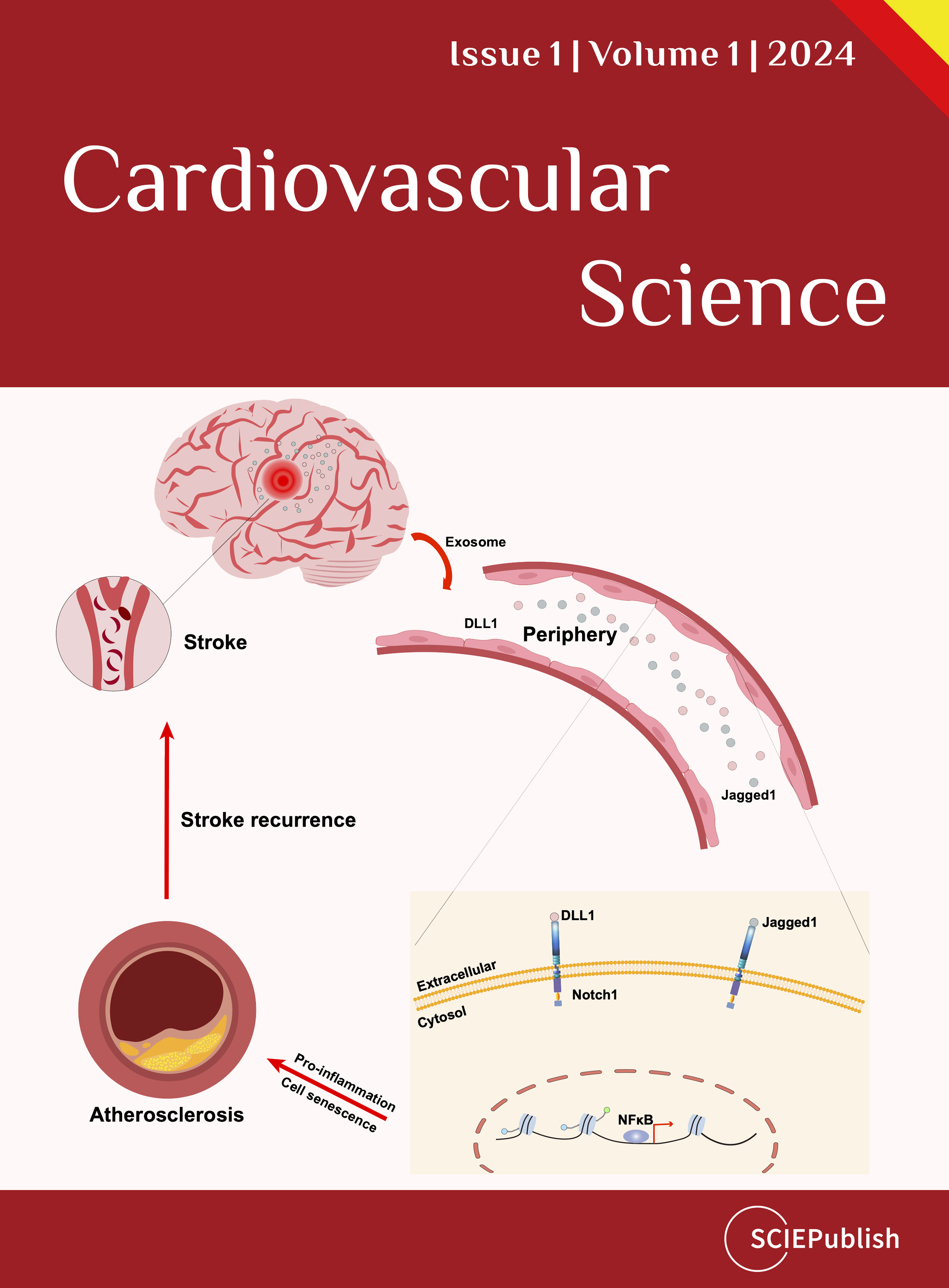
KanLi
ChenghuGuo
ShutingYu
ZekunXu
MengZhang
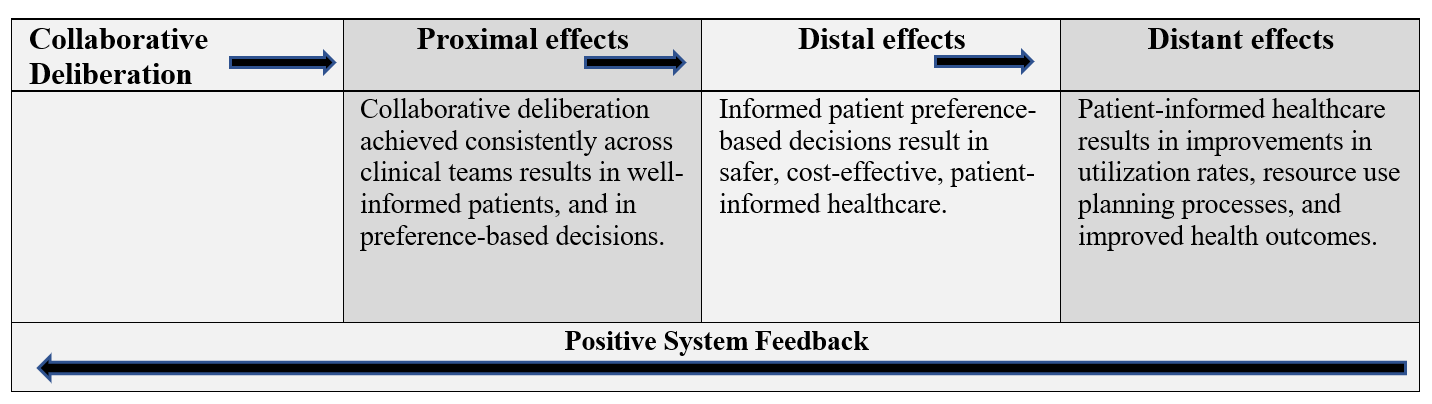
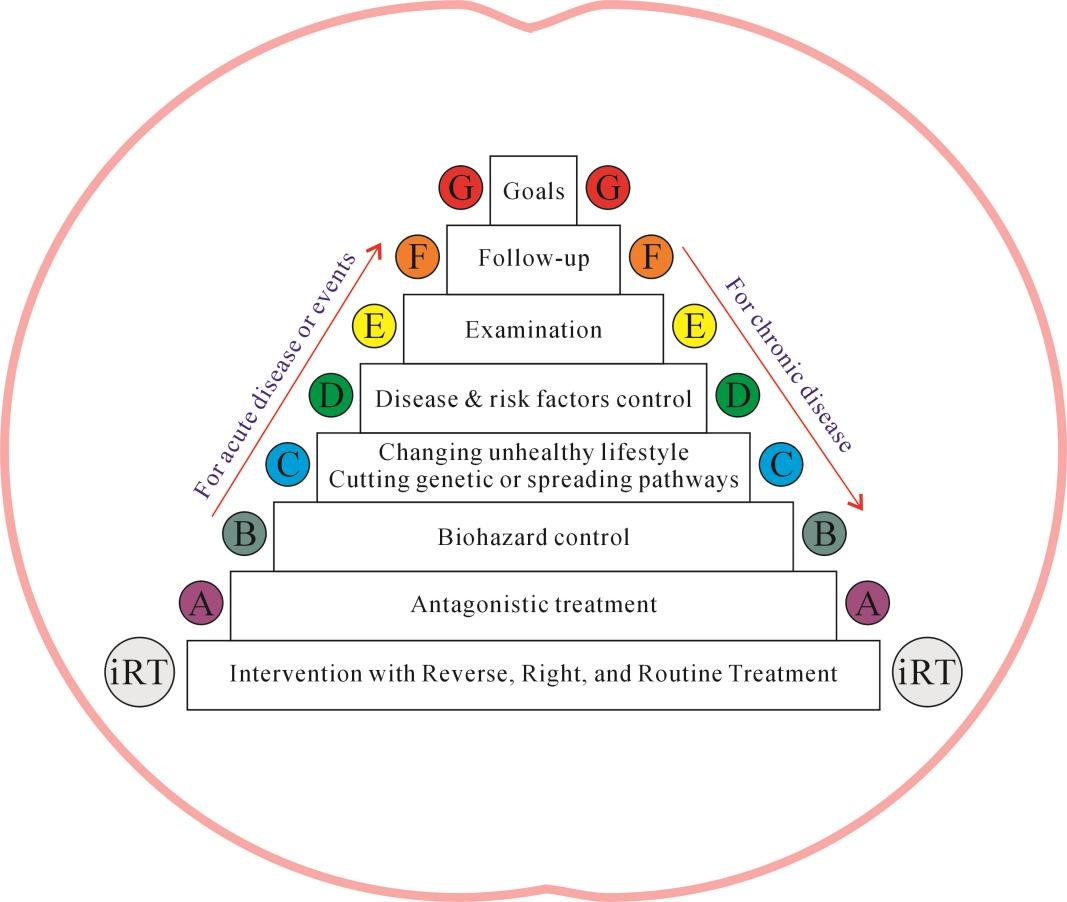
Editorial
25 January 2024
Case Report
01 April 2025
Behçet’s disease is a vasculitic condition of unknown
etiology that is characterized by oral and genital ulcers as well as various
skin and ocular lesions. Cardiovascular manifestations of Behçet’s disease are
rare, with very few cases having been reported previously in literature. We
report a case of severe tricuspid stenosis and pulmonary artery aneurysm in a
29-year-old man with Behçet’s disease, who demonstrated characteristic vascular
findings on computed tomography angiography and diagnostic valvular findings on
transthoracic echocardiogram and cardiac magnetic resonance imaging. The
patient’s Behçet’s disease was treated initially with cyclophosphamide,
azathioprine, and prednisone, which subsequently led to complete resolution of
the pulmonary artery aneurysm. As for the tricuspid stenosis, though symptoms
were managed with diuretic therapy, the severity of valvular dysfunction
required consideration and an attempt at tricuspid valve replacement surgery,
which unfortunately was met with complications and led to an unfavorable outcome
of refractory cardiogenic shock and death. Given the rarity of cardiovascular
involvement in patients with Behçet’s disease, along with the lack of clear
treatment guidelines, management of findings of tricuspid stenosis and
pulmonary artery aneurysm in these patients can be challenging.utf-8
Neibergde Alcantara Lima
Francisco FlavioCosta Filho
Euton Freitasde Castro Júnior
Shivani Reddy
Henrique Carvalho Lima Farias
GunterGerson
Ane KarolineMedinaNeri
 Open Access
Open Access